Case Study: Supporting patients living with Alzheimer's disease and their carers

Background
The Challenge
-
People living with Alzheimer’s disease often rely on daily medication to help manage symptoms like memory loss and confusion, supporting clearer thinking and daily functioning.
-
However, adherence is often compromised—especially in the first six months—due to managing side effects, confusion about dosing, and the challenges of maintaining routines.
-
Carers face the added burden of managing complex treatment schedules while providing emotional and practical support.
-
Without effective guidance, it can be difficult for both patients and carers to stay on track, making tailored support essential for improving outcomes and quality of life.
-
The mutli-component TimeTo programme was designed to address these key challenges.
Our Behaviour Change Approach
-
Using a cognitive behavioural therapy (CBT) approach along with behaviour change techniques (BCTs), each component of the programme was developed to address key behavioural barriers in Alzheimer's disease self-management.
-
Content was tailored for either the patient or their main carer as determined and nominated at enrolment.
-
The multi-component programme involved both self-directed components as well as CBT-based nurse phone calls, tailored to each patient or carer, to ensure each received relevant, meaningful support.
The Solution
Each TimeTo patient or carer received:
-
Comprehensive self-directed materials, including a welcome letter, detailed manual, feelings scrapbook, multiple medication card, patient progress report, daily activities diary, and four magazines distributed over six months.
-
Tailored CBT-based nurse support: The TimeTo patient or carer received six scheduled calls from a registered nurse over six months, providing guidance on Alzheimer’s disease, their medication, and broader disease management. A free-phone helpline was also available for inbound, ad hoc support.
The Impact
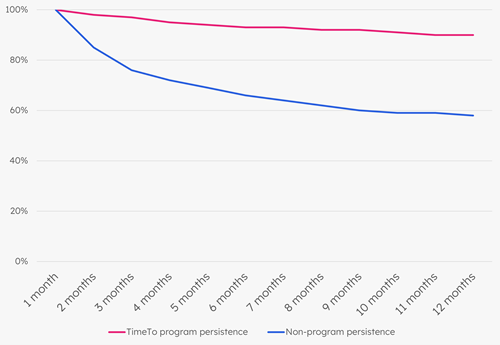
For those enrolled in the TimeTo programme:
-
90% persistence among those enrolled compared to 58% among non-programme patients at 12 months.
-
This was equivalent to a 36% increase in script fulfilment (8.3 scripts filled per year among those not enrolled in the programme vs. 11.25 scripts on those enrolled in the programme).