Perceived Medication Sensitivity Is Associated With Nonadherence
Research shows that patients have various beliefs about cancer and its treatment, which often differ from the medical understanding. It is important to understand these beliefs because they influence how patients respond to the disease, including their decision to follow prescribed treatments.
Patients' beliefs about medicine are consistently linked to whether they adhere to their medication regimen. Studies have demonstrated that assessing and changing medication beliefs can improve medication adherence.1

Research shows that patients have various beliefs about cancer and its treatment, which often differ from the medical understanding. It is important to understand these beliefs because they influence how patients respond to the disease, including their decision to follow prescribed treatments.
Patients' beliefs about medicine are consistently linked to whether they adhere to their medication regimen. Studies have demonstrated that assessing and changing medication beliefs can improve medication adherence.1
Methodology
We conducted a global online survey with 126 cancer patients who are taking self-administered anti-cancer medication at home.*
Participants answered questions about their perspectives on cancer and its treatment, including their sensitivities to medications.
We focussed on this area because many cancer patients undergo difficult in-hospital treatments before starting self-administered treatments at home. The challenges and negative experiences from past treatments can influence how patients approach their current treatment.
*More information on the demographic and clinical characteristics of the sample can be found here.
Assessing Medication Sensitivity
Participants responded to the Perceived Sensitivity to Medicines (PSM) scale2 comprised of five statements and measured using a five-point Likert rating.
Response options range from strongly disagree (1) to strongly agree (5).

Rates of Nonadherence
Using the psychometrically validated five-item Medication Adherence Rating Scale3, 56% of the sample reported at least some degree of nonadherence to their anti-cancer, at-home medication.
This is comparable to levels found by WHO and other published studies.

The Relationship Between Medication Sensitivity and Nonadherence
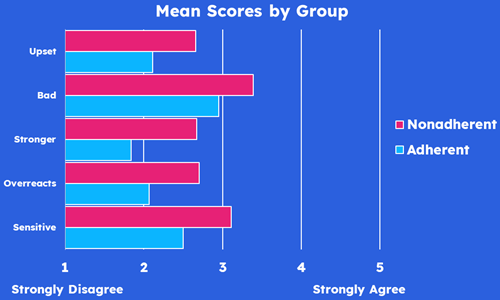
Higher levels of perceived sensitivity to medicines were reported by nonadherent participants (means are significantly higher than among adherent participants, all p < .05).
- A third of nonadherent participants endorsed the statement: “I have had a bad reaction to medicine in the past” and one in four nonadherent participants endorsed the statement: “My body is very sensitive to medicines”.
- The high frequency of endorsing these statements likely reflects patients’ negative experiences of in-hospital cancer treatments.
Improving Adherence to Self-Administered Anti-Cancer Medications
This research emphasises the importance of medication sensitivity in patients living with cancer. Those who perceive higher sensitivity to medications are more likely to be nonadherent.
These findings can be used to develop better adherence support strategies, improve health outcomes, and enhance brand and franchise value.
When a patient starts a new anti-cancer medication, their level of medication sensitivity can be easily and accurately assessed. If it is high, indicating a risk of nonadherence, interventions can be provided to help patients avoid overgeneralising past experiences to their current treatment.

Optimising Oncology Patient Support
Our findings reveal new and current insights into why people living with cancer might choose to not take their at-home anti-cancer medication as prescribed. They demonstrate the need to provide targeted and personalised patient support for those with cancer.
As part of oncology patient support programmes, interventions are required that specifically address the individual's key reasons for nonadherence. Optimising oncology patient support programmes this way will enable and empower those living with cancer to Change for Good
To learn more about how our findings can be leveraged in your patient engagement strategy, contact our Global Head of Behavioural Science and Lead Researcher—Dr Kate Perry—for a 30-minute online discussion: Click Here to contact Kate and request a meeting and receive a free copy of our study report.
Read about our expertise and more behavioural science insights.
References
1. Sheils, E., Tillett, W., James, D., Brown, S., Dack, C., Family, H., & Chapman, S. C. E. (2024). Changing medication-related beliefs: A systematic review and meta-analysis of randomized controlled trials. Health Psychology, 43(3), 155-170. doi:10.1037/hea0001316
2. Horne, R., Faasse, K., Cooper, V., Diefenbach, M. A., Leventhal, H., Leventhal, E., & Petrie, K. J. (2012). The Perceived Sensitivity to Medicines (PSM) scale: An evaluation of validity and reliability. British Journal of Health Psychology, 18(1), 18-30. doi:10.1111/j.2044-8287.2012.02071.x
3. Chan, A. H. Y., Horne, R., Hankins, M., & Chisari, C. (2020). The Medication Adherence Report Scale: A measurement tool for eliciting patients’ reports of nonadherence. British Journal of Clinical Pharmacology, 86(7), 1281-1288. doi:10.1111/bcp.14193
